Cone-beam Computerized Tomography for the Bio-mechanical Assessment of the Occipito-atlanto-axial Articulation in a 75-year-old Woman with Migraines Undergoing Blair Technique
A research article by Dr. Jonathan Verderame and Dr. Jake Hollowell
Advancing Imaging in Upper Cervical Chiropractic: Where Precision Drives Progress
Upper cervical care continues to evolve through the integration of new technologies designed to improve the way we analyze and correct misalignments at the craniocervical junction. As imaging becomes more precise, so does our ability to deliver targeted, individualized care—resulting in improved outcomes for patients with complex neurological conditions such as migraines.
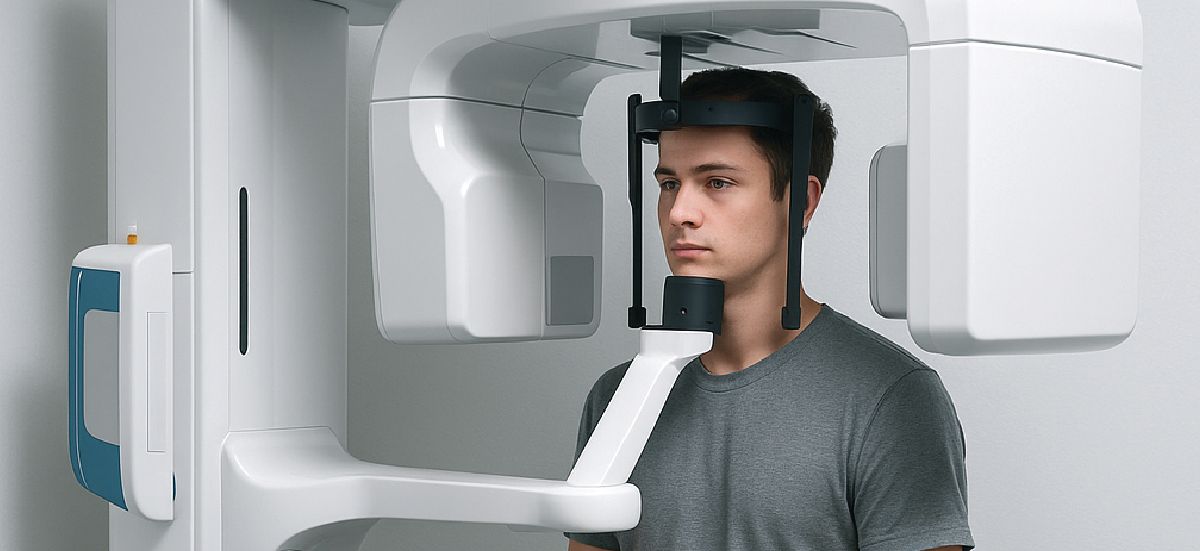
This case report by Dr. Jonathan Verderame and Dr. Jake Hollowell highlights one such advancement: the use of cone-beam computed tomography (CBCT) to guide care in a patient with chronic migraines. CBCT was utilized in place of traditional X-rays to assess the biomechanical alignment of the upper cervical spine, specifically the occipito-atlanto-axial joint complex.
The patient, a 75-year-old woman with a migraine history dating back to adolescence, received two upper cervical corrections over the course of ten weeks using the Blair upper cervical technique. These corrections were precisely directed based on detailed CBCT imaging, which revealed the directional misalignment of the atlas vertebra. By the end of the care period, her reported migraine severity had decreased significantly, and her reliance on medication was reduced.
The Broader Role of Cone-Beam Imaging in Upper Cervical Care
While CBCT is still emerging in the chiropractic profession, it has become increasingly relevant among Blair upper cervical practitioners due to its ability to capture 3D imaging without the anatomical overlap found in traditional radiographs. The Blair technique, which relies on accurate analysis of joint asymmetries between the occiput and atlas, benefits from CBCT’s ability to isolate and visualize these structures from multiple angles.
This case demonstrates how technology is shaping the next generation of upper cervical diagnostics—offering chiropractors better data, and patients more tailored care.
Staying Ahead: Imaging and Innovation at Cerebral Chiropractic Center
At Cerebral Chiropractic Center, we embrace this evolution in upper cervical care. While we do not currently use CBCT in our clinic, our existing X-ray-based protocols already provide a three-dimensional structural analysis of the upper cervical spine. This forms the basis for our Advanced Orthogonal technique—a non-invasive, sound wave-based correction system designed for precision and safety.
We are actively preparing to integrate CBCT as well as advanced imaging such as SWI (Susceptibility Weighted Imaging) and DTI (Diffusion Tensor Imaging) into our clinical model—particularly for applications like concussion and other neurological assessments. These tools allow us to continue leading with accuracy, innovation, and patient-centered care.
Read the Full Article
To explore this case in greater detail, we encourage you to read the original publication:
Cone-beam Computerized Tomography for the Bio-mechanical Assessment of the Occipito-atlanto-axial Articulation in a 75-year-old Woman with Migraines Undergoing Blair Technique.
[Access the full article here.]
Have Migraines? You Deserve Precision Care
If you’ve been struggling with chronic migraines, it’s essential to work with a specialist who can properly evaluate the structural integrity of your upper cervical spine. At Cerebral Chiropractic Center in St. Petersburg, FL, we provide imaging-based assessments and Advanced Orthogonal care designed to identify and correct the root cause of your symptoms.
If you’re looking for answers, schedule a consultation today and learn how upper cervical care may help.
More Articles